| History of Plague |
| Plague’s deadly epidemic potential is notorious and well documented. The Justinian pandemic (542 to 767 A.D.) spread from central Africa to the Mediterranean littoral and thence to Asia Minor, causing an estimated 40 million deaths. The second pandemic began in central Asia, was carried to Sicily by ship from Constantinople in 1347, and swept through Europe and the British Isles in successive waves over the next four centuries. At its height, it killed as many as a quarter of the affected population and became known as the Black Death.In the third (modern) pandemic, plague appeared in Yunnan, China, in the latter half of the nineteenth century; established itself in Hong Kong in 1894; and spread by ship to Bombay in 1896 and subsequently to major port cities throughout the world, including San Francisco and several other West Coast and Gulf Coast ports in the United States. The plague bacillus was first cultured by Alexandre Yersin in Hong Kong in 1894. In 1898, Paul-Louis Simond, a French scientist sent to investigate epidemic bubonic plague in Bombay, identified the bacillus in the tissues of dead rats and proposed transmission by rat fleas. Waldemar Haffkine, also in Bombay at that time, developed a crude vaccine.
By 1910, plague had circled the globe and established itself in rodent populations on all inhabited continents other than Australia. After 1920, however, the spread of plague was largely halted by international regulations that mandated control of rats in harbours and inspection and rat-proofing of ships. Before the third pandemic subsided, it resulted in an estimated 26 million plague cases and more than 12 million deaths, the vast majority in India. By 1950, plague outbreaks around the world had become isolated, sporadic, and manageable with modern techniques of surveillance, flea and rat control, and antimicrobial treatment of patients. From 1969 through 1993, a median of 1356 human plague cases were reported annually to the World Health Organization, with around 10 to 15 countries reporting cases each year. Plague has practically disappeared from cities and now occurs mostly in rural and semirural areas, where it is maintained in wild rodents. In the United States, the last outbreak of urban plague occurred in Los Angeles in 1924 and 1925, and human cases since then have resulted from zoonotic exposures in rural areas of western states. Plague, because of its pandemic history, remains one of three quarantinable diseases subject to international health regulations (the other two being cholera and yellow fever). The alarm that plague is still able to evoke was highlighted by the public panic over and exaggerated international response to reports of outbreaks of bubonic and pneumonic plague in India in 1994. Except for large outbreaks of pneumonic plague in Manchuria in the early part of the twentieth century, person-to-person respiratory transmission of plague during and since the third pandemic has occurred only sporadically and has been limited to clusters of close contacts of pneumonic plague patients, such as household members and caregivers. The 1994 outbreak of pneumonic plague in the city of Surat, India, although reported to be extensive, most likely involved fewer than 100 cases and 50 deaths. From 1979 through 1993, 16,312 human plague cases and 1668 deaths (mortality, 10 percent) were reported by 20 countries to the World Health Organization. In the same 15-year period, the United States reported 227 plague cases (mean, 15 cases per year) and 32 deaths (mortality, 14 percent). |
| Plague |
Category Archives: Diseases & Conditions
Plague
| Plague | ||
| Plague is one of the most virulent and potentially lethal diseases known. It is caused by an organism called Yersinia pestis.Y. pestis is a gram-negative coccobacillus in the family Enterobacteriaceae. It is a zoonotic disease and its usual hosts are rodents.It is transmitted to humans usually by flea bite and less commonly by direct contact with infected animal tissues or by airborne droplet. | ||
 |
 |
 |
| The clinical forms of plague are bubonic, septicemic, and pneumonic. Most cases are sporadic, occurring singly or in small clusters, although the potential for epidemic spread still exists in some countries.Y. pestis organism is maintained in animal cycles involving relatively resistant wild rodents and their fleas. Humans and other non-rodent mammals are incidental hosts, that is they just happen to get involved.
Transmission involving susceptible rodents and flea results in local or even widespread death of susceptible rodents and poses a more serious threat to humans. In the United States, the principal animal hosts are various ground squirrels, prairie dogs, and chipmunks. Y. pestis occasionally spills over from wild rodents to commensal rat species that inhabit cultivated fields and adjacent homes, villages, and towns. The organism can then be transported from towns to cities by these relatively cosmopolitan rats and their fleas. Plague in populated areas is most likely to develop when sanitation is poor and rats are numerous, especially the common black or roof rat (Rattus rattus) and the larger brown sewer or Norway rat (R. norvegicus). A high mortality rate from plague in these susceptible rat populations forces their fleas to seek alternative hosts, including humans. The oriental rat flea Xenopsylla cheopis and (in southern Africa and Brazil) the related species X. brasiliensis are efficient vectors of the plague bacillus among rats and are also efficient vectors to humans. |
| Except for large outbreaks of pneumonic plague in Manchuria in the early part of the twentieth century, person-to-person respiratory transmission of plague has occurred only sporadically and has been limited to clusters of close contacts of pneumonic plague patients, such as household members and caregivers. The 1994 outbreak of pneumonic plague in the city of Surat, India, although reported to be extensive, most likely involved fewer than 100 cases and 50 deaths. |
| Plague can be transmitted during the skinning and handling of carcasses of wild animals such as rabbits and hares, prairie dogs, wildcats.Carnivores, including dogs and cats, can become infected with Y. pestis by eating infected rodents and perhaps by being bitten by fleas from infected rodents. Although clinical plague commonly develops in infected cats, it rarely does so in infected dogs, which thus do not directly expose humans to infection. However, both dogs and cats may transport infected fleas from rodent-infested areas to the home environment. |
|
Clinical Features |
| Plague is characterized by a rapid onset of fever and other systemic manifestations. If it is not quickly and correctly treated, plague can follow a toxic course, resulting in shock, multiple-organ failure, and death.In humans, the three principal forms of plague are bubonic, septicemic, and pneumonic. Bubonic plague, the most common form, is almost always caused by the bite of an infected flea but occasionally results from direct inoculation of infectious tissues or fluids. Septicemic and pneumonic plague can be either primary or secondary to metastatic spread.
Bubonic plague usually has an incubation period of 2 to 6 days, occasionally longer. The patient experiences chills, fever; myalgias; arthralgias; headache; and a feeling of weakness. Soon usually within 24 h the patient notices tenderness and pain in one or more regional lymph nodes proximal to the site of inoculation of the plague bacillus. Because fleas often bite the legs, femoral and inguinal nodes are most commonly involved; axillary and cervical nodes are next most commonly affected. The enlarging bubo becomes progressively painful and very tender. The surrounding tissue often becomes oedematous, sometimes markedly so, and the overlying skin may be erythematous, warm, and tense. Inspection of the skin surrounding or distal to the bubo sometimes reveals the site of a flea bite marked by a small papule, pustule, scab, or ulcer. Septicaemic plague is a progressive, overwhelming bacterial infection. Primary septicemia develops in the absence of regional lymphadenitis. Patients with septicemic plague often present with gastrointestinal symptoms of nausea, vomiting, diarrhea, and abdominal pain. If not treated early with appropriate antibiotics, septicemic plague can be fulminant and fatal. Pneumonic plague develops most rapidly and is most frequently fatal. Pneumonic plague arises from exposure to infective respiratory droplets from a person or cat with respiratory plague or secondary to hematogenous spread in a patient with bubonic or septicemic plague. Pneumonic plague can also result from accidental inhalation of Y. pestis in the laboratory. The incubation period for primary pneumonic plague is rarely longer than 1 to 4 days. The onset is most often sudden, with chills, fever, headache, myalgias, weakness, and dizziness. Pulmonary signs, including cough, sputum production, chest pain, tachypnea, and dyspnea, typically arise on the second day of illness and may be accompanied by haemoptysis, increasing respiratory distress, and circulatory collapse. Prevention A killed, whole-cell plague vaccine is available in the United States. Primary immunization consists of a series of three injections followed by booster doses as warranted (at intervals of 6 months or more) Treatment Streptomycin is the drug of choice. Alternative antibiotics include the Tetracyclines and Chloramphenicol. |
| History of Plague |
Psoriasis ~ Treatment
| Psoriasis ~ Treatment | |
| Although there is no known cure of psoriasis, the disease can be effectively controlled by various treatment modalities.The mainstay of topical treatment of psoriasis is coal tar which was made popular by Goeckerman in 1925. Used for 8-10 hrs. (1%,5%,25%) is very effective.Majority of the patients respond to topical therapy which includes emollients, keratolytics, coal tar, anthralin and corticosteroids. The newer agents are topical PUVA, Topical Methotrexate, Calcipotriol and Tazarotene (a retinoid).Coal Tar preparations: 100 % strong coal tar solution and 4 % tar paste are to be applied to the patches twice daily. Salicylic acid 1-2 % may be added to the preparation to remove scaling. Dithranol: 1-2 % dithranol cream is applied to the lesions for duration of 30 minutes daily. Coal tar and Dithranol preparation are best avoided on face, genitals and skin folds as they are irritating. Topical Steroids: Their long term use is not indicated in most cases as on their withdrawal relapse may occur and the disease may change to unstable phase. Indications of their use are lesions of face, genitals and skin flexures where coal tar may be too irritant. Unresponsive lesions of scalp and soles may also need topical steroids. Ultraviolet radiation: Natural sunlight has beneficial effect. During winters medium wave ultraviolet radiation is helpful. Systemic treatment: In extensive psoriasis which fails to respond with local measures may need to be put on systemic treatment considering the side effects as they have to be taken for long period. Psoralen, Retinoids (etretinate), Methotrexate have to be given along with local medication. |
|
| METHOTREXATE is a Most-effective treatment of psoriasis that is widespread, covering large areas of the body, and resistant to conventional topical therapy, according to Dr. Inderjeet Kaur, Associate Professor, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh.In 82 selected patients with psoriasis at the PGI, methotrexate (MTX) led to clearance of the lesions in nearly 80% in a mean period of 8 weeks, Dr. Kaur said in the Fulford oration at the 26th annual conference of the Indian Association of Dermatology, Venereology and Leprology.With the stringent precautions taken, MTX therapy did not provoke adverse side effects such as hepatotoxicity, even when used in children and elderly patients to control severe disease episodes. | |
| Palmo Plantar PsoriasisTreatment of PPP which causes severe handicaps both cosmetically and functionally presents particular challenge.MTX gel 1 % was used twice daily for 8 wks. Good improvement was found in 80% of palmar and 64% of planter lesions. Topical MTX if used in a suitable vehicle that enhances percutaneous absorption and if used for a sufficient length of time has beneficial effect on PPP. |  |
| Topical PUVASOL : The palms and soles of the patient was submerged in an 8-MOP soak solution for 15 minutes, followed by sun exposure immediately after drying. The treatment was given twice weekly for 8 weeks. 70 % palmar and 27 % planter cases show good improvement. Only one patient had phototoxic reaction. PUVASOL is effective and safe therapy for palmar psoriasis.Coal – tar therapy: 6 % crude coal tar (CCT), when used under occlusion, resulted in good improvement in 77 % of PPP patients.Calcipotriol: Calcipotriol ointment 50 micg/g was used every night under occlusion for 8 weeks. Excellent improvement was seen in the palms. |  |
|
Systemic Treatment Systemic treatment is reserved for patients with extensive disease or on whom conventional therapy has failed. Systemic therapy include PUVA, Conticosteroids, MTX, Hydroxyurea, Cyclosporine and Calcipotriol. Before starting systemic therapy, patients undergo complete clinical and laboratory evaluation and only those with near normal renal, hepatic and marrow function are selected to receive MTX. In the PGI series, 82 patients were given a single oral weekly dose of 0.4-0.6 mg/kg body weight of MTX. Nearly 80% clearance was seen in a mean period of 8 weeks. The drug could he completely withdrawn in 90% patients, coinciding with the seasonal remission. There was no response in 2 patients. The commonest side effects were nausea and vomiting, which occurred in 30% patients. Post- MTX disease free interval was 7.7 months. The drug had to be restarted in 13 patients while the others could be managed with topical therapy in the subsequent relapses. MTX-free period of 4-6 months reduces the drug’s hepatoxicity. MTX has also been used safely and effectively in children and elderly patients to control severe episodes of the disease. |
|
|
Other systemic drugs tried included Mesalazine, effective in about one-third of the patients, oral Nystatin, found to be ineffective, and cyclosporine, used in selected cases to tide over a crisis. Corticosteroids were found to have no role in routine treatment of psoriasis because of the risk of rebound. |
|
| FDA OKs mousse to treat psoriasis Patients who suffer psoriasis of the scalp won a slightly different kind of treatment a mousse-like foam to rub onto scalp lesions with less mess than traditional drugs. Until now, the main treatment has been a lotion containing the chemical betamethasone, but putting a lotion on the scalp every day is messy and greasy. The Food and Drug Administration approved Connetics Corp.’s new version of betamethasone, an easier-to-apply foam called Luxiq. An estimated 3.5 million Americans have scalp psoriasis, marked by redness, scaling, severe itching and irritation. In one study of 172 patients, 72% treated with Luxiq had complete or almost complete clearance of their psoriasis outbreak, compared with 47% who used a betamethasone lotion. |
|
Psoriasis
| Psoriasis | |
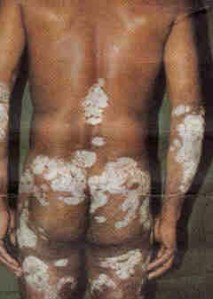
| Psoriasis is non infectious, inflammatory disease of the skin. It is characterised by well defined erythematous plaques with adherent silvery scales. |  |
| 1-3 % of the population has this disease. More common in Europe and North America.Often seen between 15 to 40 yrs. |  |
| Aetiology Real aetiology is unknown. Genetic: If one parent is affected the offspring has 25% chance to develop the disease. If both parents are affected the chances rise to 60%.The disease has been found to have a genetic basis. On HLA phenotyping of the Chandigarh patients, a positive association was seen with HLA-B17 . However, familial occurrence was detected in only 2%. |  |
| Common Patterns of Psoriasis:
Plaque pattern: It is the most common type. The individual lesions are well demarcated and are red with dry silvery white scaling. Most common sites involved are scalp, elbow, knee and lower back.
|
 |
| Geographical tongue seen in 3.8% and Blepharitis in 5%. |  |
| Scalp: This site is often involved. Areas of scaling are inter-spread with normal scalp. Significant hair loss occurs only if there is gross involvement. Nails: Involvment of nails is common. Thimble pitting, Onycholysis (separation of nail from nail bed), Subungal hyperkeratosis are main changes seen in the nails. Involvement of nails reflect the extent of the disease elsewhere. Flexures: Involvement of flexures like axillary folds and submammary folds are not scaly but red, glistening and symmetrical. Palms: Psoriasis in the palms is poorly demarcated and is poorly erythematous. |
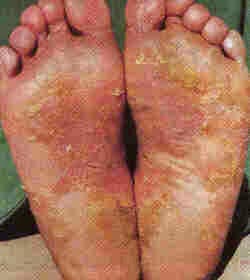 |
| Less common types of psoriasis are Napkin psoriasis and Localised pustular psoriasis in the palms and soles consisting of numerous small sterile pustules on erythematous base. | 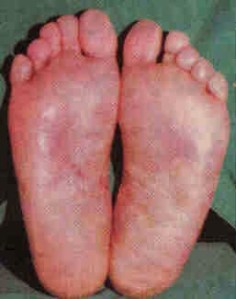 |
| Complications: Psoriatic Arthropathy is seen in 5 %. There may be distal small joint involvement mainly terminal interphalangeal joints of hands and toes. Single large joint arthropathy may also be seen which mimmics rheumatoid arthritis. Sacroiliac joint and lumbar spine involvement may also be seen. |  |
| Serum copper levels are found to be higher while serum zinc levels were lower in Psoriatics as compared to controls.Urinary tract cell counts were significantly higher in Psoriatics. |  |
| Psoriasis ~ Treatment | |
Premenstrual Syndrome
| Premenstrual Syndrome |
Premenstrual Syndrome consists of variety of symptoms that occur during a particular phase of menstrual cycle, usually 7-10 days before the periods begin. cycle, usually 7-10 days before the periods begin.These symptoms mostly begin in 20s. 10 to 50 % of women suffer from PMS regularly. 5-10 % suffers from symptoms severe enough to seek medical help. Women most often affected by PMS are those:
PMS is rarely debilitating. |
| Symptoms Of PMS occur 7-10 days before periods are due. | More intense symptoms in a small number of women |
|
|
CausesNumerous theories are proposed to explain the symptoms of Premenstrual Syndrome.
|
Treatment
Various relaxation techniques, such as yoga and meditation, can be helpful in reducing the anxiety, irritability and other emotional symptoms that sometimes occur premenstrually. The Cobra and Bow yoga positions are particularly recommended for PMS. Hormonal agents, anti-anxiety and antidepressants may be needed in some. |
| Calcium most helpful in Premenstrual syndromeOf all the dietary supplements that claim to help women reduce the physical and emotional symptoms associated with premenstrual syndrome (PMS), there is only one that is really helpful – calcium.
Researchers say there is convincing evidence that 1,000-1,200 milligrams/day of calcium can substantially reduce PMS symptoms such as fatigue, irritability and abdominal bloating. Magnesium supplements of 200-400 mg/day may be helpful, but their efficacy hasn’t been proven and higher dosages can trigger a mild laxative effect. Other supplements, including vitamin B6, have conflicting results in past studies, according to a report in the Journal of the American College of Nutrition. Other remedies supposed to benefit PMS are chaste tree oil and dong quai. These herbs may be unsafe for women who become pregnant. No scientific evidence has proved their effectiveness. So, if one is looking for something to help with PMS, calcium tablets are the best bet. Cutting down on fat in your diet also helps. |
