| Migraine | ||||||||||||||||||||
| Migraine is an episodic unilateral headache accompanied by visual disturbances and vomiting. The episodic nature of the headache is most characteristic. Initially during aura, there is a decrease in cerebral blood flow, particularly in the occipital and parietal lobes. Later, during the phase of headache there is a dilatation of the extracranial arteries related to the variations in 5-HT blood levels.Types of Migraine1. Classical migraine: The headache is preceded by visual or sensory aura.2. Common migraine: This is without aura. Headache, nausea, vomiting and photophobia are the classical symptoms.3. Hemiplegic migraine: In this type, hemiplegia lasting for a few days follows the headache.
4. Basilar migraine: Vertigo, diplopia, dysarthria with or without visual symptoms precede occipital headache. 5. Cluster headache: Bouts of severe pain around one eye with associated epiphora and nasal congestion is the hallmark and this type, mostly affects males. Treatment Treatment of migraine involves managing acute attacks with analgesics and prevention of further attacks. Precipitating causes have to be taken care of and family and work related stress should be managed by various methods of coping with stress and relaxation and keeping regular hours of sleep and meals habits. Simple analgesics like asprin, acetoaminophen and also ibuprofen and diclofenac are used to alleviate pain. Ergotamine is used when analgesics give less relief. It acts by causing vasoconstriction of extracranial vessels and reduction of platelets aggregation. Sumatriptan is a highly selective 5-HT1 receptor agonist which are mainly located in cerebral arteries. It constricts cerebral blood vessels. Dopamine antagonists, metoclopramide, chlorpromazine, prochlorperazine have been used for severe attacks. Narcotics and short course of corticosteroids and antipsychotics can be used when severe migraine does not respond to conventional measures. Precipitating Factors Although investigation have not conclusively proved that any factor causes migraine headache, some patients do recognize certain factors that precipitate an attach. Certain dietary factors like Tyramine, monosodium glutamate, excessive alcohol, excessive analgesics, ergotamine, and oral contraceptives act as trigger to cause migraine. Diagnosis: Careful history is important. Diagnostic criteria Migraine without aura A. At least 5 attacks fulfilling criteria B-D B. Headache attacks lasting 4-72 hours (untreated or unsuccessfully treated) C. Headache has at least 2 of the following characteristics:
D. During headache at least 1 of the following:
E. Not attributed to another disorder Migraine with aura A. At least 2 attacks fulfilling criterion B B. Migraine aura fulfilling criteria B-C for one of the subforms (typical aura with migraine headache, typical aura with non-migraine headache, typical aura without headache, familial hemiplegic migraine, sporadic hemiplegic migraine, or basilar-type migraine) C. Not attributed to another disorder Typical aura with migraine headache A. At least 2 attacks fulfilling criteria B-D B. Aura consisting of at least 1 of the following, but no motor weakness:
C. At least two of the following:
D. Headache fulfilling criteria B-D for “Migraine without aura” begins during the aura or follows aura within 60 minutes E. Not attributed to another disorder Typical aura without headache As “Typical aura with migraine headache” except: B. Aura consisting of at least 1 of the following, with or without speech disturbance but no motor weakness:
D. Headache does not occur during aura nor follow aura within 60 minutes Prevention of Migraine Preventive measures are to be considered when migraine attacks occur more than two or three times a month and disturb normal activity. Preventive medication is continued for 6 months and gradually withdrawn. Drugs used include 5-HT influencing drugs like Amitriptyline, Methysergide, Propranolol, Metoprolol, Nadolol, Nefedipine, Nimodipine,Verapamil, Pizotefen. |
||||||||||||||||||||
Drugs used in Migraine
|
Category Archives: Diseases & Conditions
Melatonin
| Melatonin |
| Melatonin is a hormone secreted by the pineal gland. The pineal gland is a pea like structure located in the centre of the brain. What is now known is that it is part of the body clock, an internal timer that regulates the production of various hormones which in turn control human activities like – sleeping, eating, sexual development, immune systems and maternal instincts.Plasma Melatonin levels increase steadily between 9 p.m. and 11 p.m. and reaches its peel value between 2 a.m. and 4 a.m. The level of this hormone then declines and reaches its low level in the afternoon.
Melatonin is synthesized by the pineal gland from the neurotransmitter, serotonin. Serotonin is involved in several central physiological processes, including body temperature and blood-pressure regulation, as well as a variety of neuro-psychological functions such as appetite, memory, and mood. Melatonin and serotonin are inextricably linked: When melatonin levels drop or rise for any reason, so do serotonin levels, and vice versa. Actions of Melatonin
Taking Melatonin Why take Melatonin ? There is lot to be learned about Melatonin. Research is underway to determine melatonin’s effects on human body and its more precise role and actions. Recommended dose: It varies between 100 mcg to 200 mg. Start with lower dose and increase gradually. It is one of the least toxic substances. Those taking Prozac should not take melatonin. Melatonin should not be combined with Vitamin B6. It should also not be combined with oestrogen or any other hormone. When should melatonin be taken: Melatonin should only be taken at night-time, usually about thirty minutes prior to going to bed. If you are travelling on a long trip you may want to take a low dosage 300mcg tablet prior to getting on your flight. |
Molluscum Contagiosum
| Molluscum Contagiosum | |
| Molluscum contagiosum is a skin disease. It is generally a benign disease characterized by pearly, flesh-colored, umbilicated skin lesions 2 to 5 mm in diameter. It is caused by a Poxvirus. The infection can be transmitted by close contact, including sexual intercourse. Lesions typically occur in the genital region but can be found anywhere on the body except the palms and the soles. In most cases the disease is self-limited and has no systemic complications. |
 |
| Mulluscum contagiosum develops often in cases with the advanced stages of HIV infection. 5 to 18 percent of HIV-infected patients develop this complication. The disease is more generalized and severe in AIDS patients with frequently involving the face and upper body. | 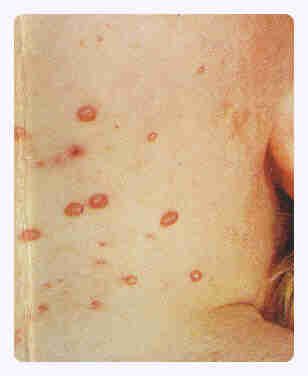 |
| There is no specific systemic treatment for molluscum contagiosum, but a variety of techniques for physical ablation have been used such as Electocautry, chemical cautry, Trichloroacetic acid applications or Liquid nitrogen applications or Light electrosurgery. |  |
| Skin Diseases | |
Menorrhagia
| Menorrhagia ~ Excessive Menstrual Bleeding |
| It is one of the most common menstrual disorders and is called Menorrhagia. It affects about a third of the women. A woman who bleeds for more than 10 days or women who uses more than 10 pads a day may be labelled as suffering from Menorrhagia.
Causes:
Women due to excessive bleeding develop anaemia. It leads to deterioration of general health which lead affects family and social life. Dysfunctional Uterine bleeding is abnormal uterine bleeding caused by interruption of normal ovarian functions that produces eggs called ovulation. Tests are performed to evaluate the status and cause of the bleeding. These include blood tests, ultrasound examination, Pap smear, D&C, and Hysteroscopy. Women who experience single episode of heavy bleeding may not need much treatment but those who get heavy bleeding for more than 24 hrs need to seek medical advice. Relief from menorrhagis is achieved by treating under lying causes. Often it is managed with progesterone or a combination of progesterone and oestrogen as in the form of oral contraceptive. |
Hormone Replacement Therapy (HRT) ~ Risks
| Risks of Hormone Replacement Therapy (HRT) |
| Two major studies created lot of the furrow and confusion among a large population of women and medical professionals. The first, Women’s Health Initiative (WHI), was called off after Prempro, a popular estrogen and progesterone combination therapy, was shown to increase risk of stroke, heart disease and breast cancer in post-menopausal women.The second, being conducted by the National Cancer Institute (NCI), showed that post-menopausal women who took estrogen had a 60 percent greater chance of contracting ovarian cancer than did women who took no hormones.
Estrogen products have been used for decades and have helped millions of women handle symptoms of menopause, including hot flashes, night sweats, sexual discomfort and the increased risk of bone fractures. For years, studies on heart disease, Alzheimer’s, colon cancer and bone fractures also showed potential benefits to women taking hormone replacement long-term, and these findings were widely accepted by doctors and advertised by the drug makers. The findings regarding the benefits of estrogen on heart disease were considered strong enough by the American Heart Association to be included in its literature for women as recently as 1997. But all this has changed over night with the findings of WHI. Researchers running the federally funded Women’s Health Initiative announced that the largest U.S. trial of combination hormone therapy in healthy postmenopausal women had been stopped three years early because of an increase in breast cancer cases among hormone users. Increases in heart attacks, strokes and blood clots also led the oversight committee to halt the study. Overall, the researchers concluded that the treatment was hurting the test subjects more than it was helping them. That assessment applied to women taking estrogen and progestin, but not to women in a separate study evaluating the use of estrogen alone. Researchers said that they had not detected any significant increase in breast cancer among women taking estrogen only and that the study would continue. Experts say, women who are taking the hormones should not panic, but should consult with their doctors about whether to continue. It is advised that women who take the two hormones to relieve hot flashes and other symptoms of menopause should use the treatment as briefly as possible, and those wishing to prevent osteoporosis should probably choose alternatives to hormones. Also, the result of this study on the use of contraceptive is unclear for the present. The observations of this study has no bearing on the use of contraceptive pills by women of pre menopausal age. This study was conducted with Prempro. Prempro is taken all month, while oral contraceptives are prescribed to be taken for three weeks, then stopped for one week — to mimic the body’s natural hormonal cycle. Some think this cycling may be protective. |
| Findings of WHI in relation to HRT |
Following are the observations out of the Women’s Health Initiative study:Before stopping its eight-year study at the five-year mark, the WHI came to the following conclusions:
There was no difference in death rates between the two groups. However, women on the hormone treatment had a
In contrast, the hormone-treated women
The study found that the frequency of these effects in hormone users did not differ by age, ethnic group or prior health status. |
