| Tumescent Liposuction |
| The Tumescent Technique, which permits the local anesthesia of large areas of subcutaneous fat, was developed by a California dermatologic surgeon Jeffrey Klein, M.D., in 1985. Klein first presented his findings in 1986 at the Second World Congress of Liposuction Surgery in Philadelphia. The Tumescent Technique utilizes large volumes of saline solution, containing dilute local anesthetic and adrenaline, which is injected into the fatty tissue. The injected area then becomes locally anesthetized – “numbed”. There may be some discomfort during the initial process of injection. With the tumescent technique, liposuction patients usually need no general anesthesia, as compared with the traditional standard liposuction methods. However, patient may require intravenous sedation or narcotics. In fact, many receive only minor sedation to help them relax, and are completely conscious and comfortable during suctioning portion of tumescent liposuction surgery. After surgery, most patients may get up and walk out of the office without assistance. Patients are usually back to their regular routine in a couple of days. With the Tumescent Technique, postoperative discomfort is significantly reduced, since the local anesthesia remains in the treated tissue for 16 hours after surgery.The Klein formula tumescent solution is injected into the fatty tissue through small, “numbed” slit incisions in the skin. These slit incisions are made, when possible, in inconspicuous places. The tumescent fluid is injected under pressure which causes the target fatty tissue to become firm and inflated. This allows the surgeon to later extract the fat in a more accurate and uniform fashion, thereby producing smoother results. The anesthetic and other agents in the tumescent solution should be allowed sufficient time to diffuse (percolate) and take full effect throughout the fatty tissue. The solution will numb the areas as well as reduce bleeding by temporarily closing down capillaries. Constricting the capillaries is important to reduce bleeding during and after surgery. Less bleeding means less bruising. Not only does this make the surgery safer, it also speeds up postoperative recovery. As a result, most patients can return to work or their regular routines in a couple of days. |
Advantages of Tumescent Liposuction
|
Obesity Liposuction

 large amount of weight within a few days without toiling hard.
large amount of weight within a few days without toiling hard.

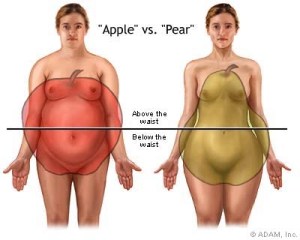
 attacks based on your body shape.If your waist-hip ratio is 0.72 to .76 and you are under 60, your risk is 1.7 times higher than the standard or 70 percent higher.If your ratio is 0.76 to 0.80, your risk is two and a half times higher.If your ratio is 0.80 to .88, your risk approaches three times higher.If your waist-hip ratio is over 0.88, your risk is four and a half times higher.If you are older than 60, the top category of risk is 1.9 times higher.So you can see that the effects of this are diminished in women over the age of 60, implying that extra abdominal fat is less risky for older woman. Now here is the major point of this study. With minor exceptions, it didn’t matter whether your body mass index was under 25 or over 25. In other words, an overweight woman, if she has more of an hour-glass figure, seems to be protected. In addition, you can look at the absolute waist circumference measurements.
attacks based on your body shape.If your waist-hip ratio is 0.72 to .76 and you are under 60, your risk is 1.7 times higher than the standard or 70 percent higher.If your ratio is 0.76 to 0.80, your risk is two and a half times higher.If your ratio is 0.80 to .88, your risk approaches three times higher.If your waist-hip ratio is over 0.88, your risk is four and a half times higher.If you are older than 60, the top category of risk is 1.9 times higher.So you can see that the effects of this are diminished in women over the age of 60, implying that extra abdominal fat is less risky for older woman. Now here is the major point of this study. With minor exceptions, it didn’t matter whether your body mass index was under 25 or over 25. In other words, an overweight woman, if she has more of an hour-glass figure, seems to be protected. In addition, you can look at the absolute waist circumference measurements.