| Prevention & Treatment of Osteoporosis |
| The Role of Hormone Therapy (HRT) in the Prevention and Treatment of OsteoporosisWhat is Hormone Therapy?
Hormone therapy in cases of osteoporosis is treatment which supplements of the hormones that ovaries have stopped making at menopause. It consists of either Oestrogen alone or in combination with Progesterone. |
Possible guidelines for the use of Hormone therapy
|
| Types of Hormone therapy Hormone therapy can be given in a number of ways. Oestrogen can be given alone or in combination with progesterone. When oestrogen is given alone chances of uterine cancer increases. To eliminate this risk progesterone can be added to oestrogen. Women who have had a hysterectomy may be treated with estrogen alone.Common Hormone Regimens
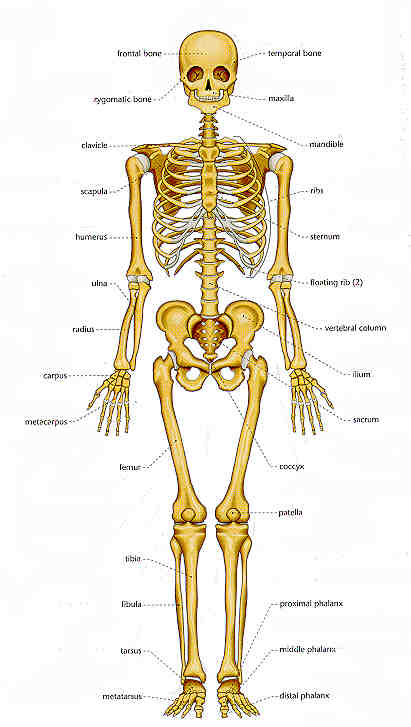
Recently claims have been made that natural progesterone creams will prevent osteoporosis. A dosage of 0.625 mg of oral estrogen per day (or its equivalent) is the minimum dose required to protect against osteoporotic fractures. Lower doses of estrogen (0.3 mg per day) combined with calcium supplements (1,500 mg per day) may also protect bones. Side effects of Hormone therapy: depression, headaches, breast tenderness, skin irritation and weight gain. |
Conditions when Hormone therapy is to be Avoided
To be on Guard when on Hormone therapy
|
| Other benefits of Hormone TherapyResearchers believe it helps to prevent heart disease; and it may provide protection against Colon cancer, Alzheimer’s disease and stroke. |
| Risks of Hormone therapyMost researchers believe that hormone therapy is safe for short term – 10 years. Even for longer use the risks are minimal and the benefits outweigh the risks.
Results of various studies suggest that over a lifetime approximately 10 in 100 women on hormone therapy will develop breast cancer. |
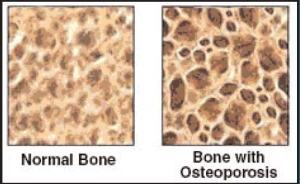
| Osteoporosis |
Prevention & Treatment of Osteoporosis
Reply